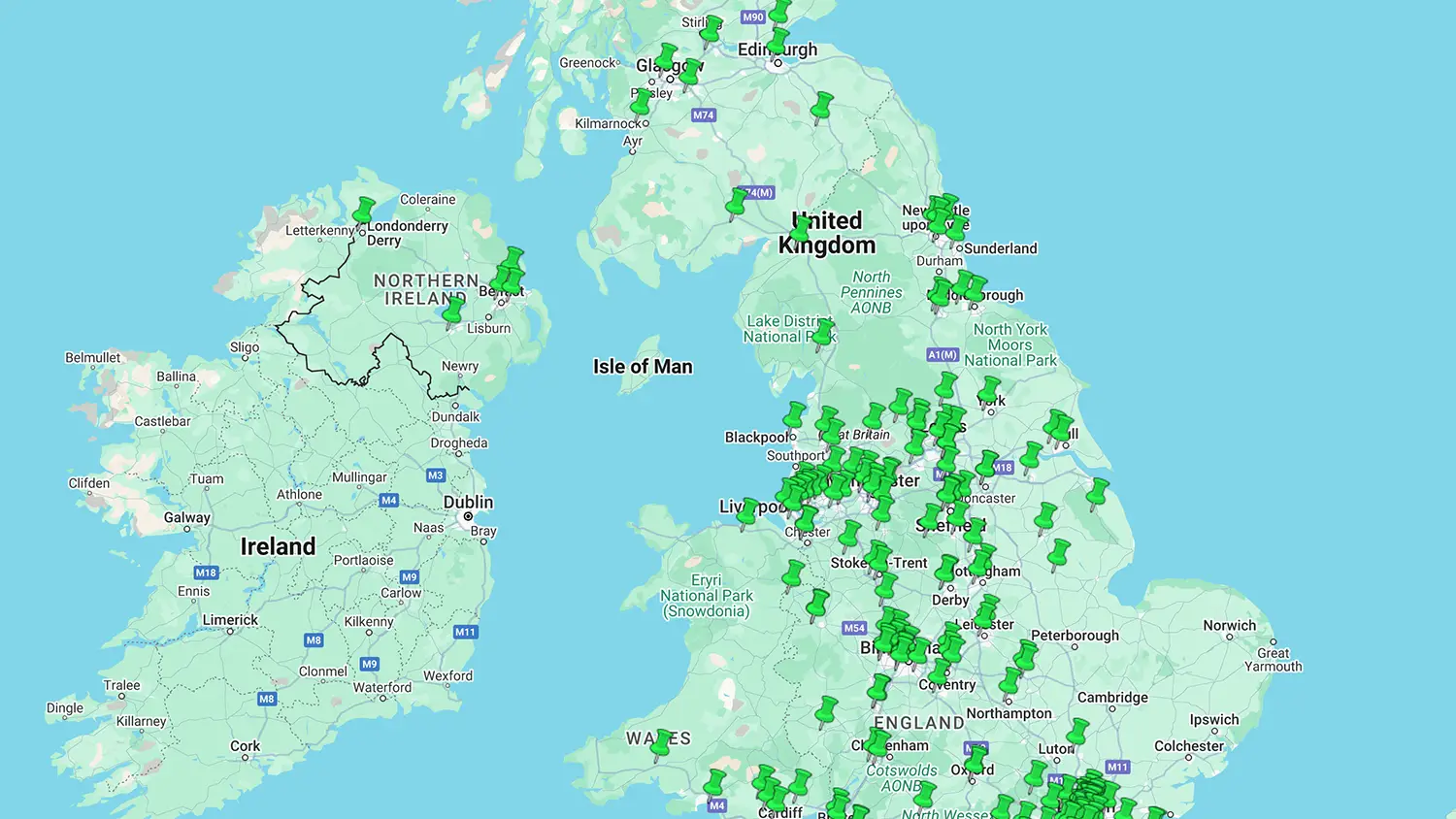
Today, NMCWatch is releasing a unique set of data on the number of fitness to practice (FtP) referrals by NHS Trusts to the Nursing and Midwifery Council (NMC). This data is the result of multiple Freedom of Information requests made over many months. It is presented as both a UK map showing each trust’s location and as a dynamic spreadsheet.
Why we collected this data
Since 2017 NMCWatch has made dozens of Freedom of Information requests (FOIs) to the NMC to clarify many regulatory issues. FOIs are an essential tool for collecting information on the FtP process. Registrants being investigated are often removed from their workplace and can find it difficult to obtain information to support their case.
Information gathered during FOIs helps give context to a referral. Our requests vary from the number of referrals from a particular employer (which helps us understand a member’s case if we find that their employer refers large numbers of registrants) to information about specific details of the fitness to practice process. We also know that the NMC referral process allows fitness to practice to be weaponised to punish good registrants who may, for example, have raised concerns in their workplace.
By collecting this data, we now have the undeniable facts to back up the years of anecdotal evidence we have of a fitness to practice process that we believe is not fit for purpose.
Poor management or lack of willingness to change?
In 2019, Andrea Sutcliffe announced changes to move towards a more person-centred approach to FtP investigations. The Ambitious for Change project set about addressing different aspects of FtP. Each region was allocated their own NMC “Principle regulation Advisor” who could be approached for advice on potential referrals but would also work to educate and support centres in resolving issues at a local level. The hope was that referrals would only then be received after a localised disciplinary and investigation procedure found an ongoing risk.
In May 2022 the NMC expanded their employer link service. Internal NMC audits did indeed show that many referrals could have been dealt with locally. So the service offers local solutions to enable this, and further reduce the FtP case backlog. A referral support line was established as well as the independent CIC Careline for registrants undergoing FtP referral.
The employer link service initially reduced employer referrals for FtP cases “by 50%” between 2020-22, showing the potential for success this project had (Open Council 26th May 2022 – top of page 9). However, this effort is seemingly undone with the admission in their annual fitness to practice report for 2023 – 24 (Foreword, p5, para 3) that the NMC failed to reach the target of 4000 cases (PSA standard 15). Their reasons included the substantial increase in referrals which was discussed further in this Nursing in Practice article.
Following the independent report by Rise Associates this year, £30 million was allocated to start extensive work on reducing the backlog. Sadly, the teams previously allocated to the successful employer link service have now been moved over to the teams dealing with the backlog. Reports appear to show (page 49 of papers for 24 September 2024 Council meeting) that more resources were being allocated to commence this workstream, but no more staff have been recruited, instead, they have been moved (ELS Annual report pages 127 – 164) from other productive teams such as the employer link service. Will this mean inappropriate employer referrals begin to rise again?
The data does not lie…
We have been collecting data from all 223 trusts and health boards across the UK to determine the number of FtP referrals they make. 42 initially refused to engage, often stating they had no centralised system of recording the numbers of nursing or midwifery staff referred to the NMC. Considering the impact this can have on registrant safeguarding and the public safety aspect of needing to learn from lessons involving the necessity to refer (Morecambe Bay, etc), this is concerning.
With the assistance of the Information Commissioners Office many of these trusts were persuaded to try harder to provide the data so that as of today, all but seven have responded. Others have attempted to avoid full disclosure but are again being encouraged by the ICO that partial disclosure on the grounds of confidentiality is not acceptable. Data from those nine trusts or boards is expected.
Even more worrying is that there is often a disparity between the number of registrants a trust states it has referred and the number the NMC states it has received from the trust. The NMC has difficulty answering requests about the number of registrants a particular trust or employer has referred and seems even less able to demonstrate any themes between those trusts or employers that have high numbers of referrals.
A further FOI to the NMC requested information on engagement by NHS trusts and the employer link service. This was refused by the NMC as it was determined that
“Section 12 of the FOI Act allows public bodies to refuse a request if it is estimated that it would take over 18 hours or, would exceed a cost of £450 to compile the information to answer, this is known as ‘exceeding the appropriate limit”.
We suspect the true answer is that no cogent data has been collected to date. This is despite pledges to invest significant finances to improve the IT systems at the NMC for a number of years.
Our questions are simple:
- Why does the NMC not gather this data routinely?
- Why does the NMC not audit the employer link service with robust lessons learnt reflected back to the FtP process?
- Why does the NMC not escalate when an employer refers high numbers of registrants to identify potential risk to the public?
- When there are clear links between employers with high referrals to the NMC and published poor care, why is the NMC not doing more to utilise the intelligence they gather through referrals to identify potential “danger zones” and coordinate with other authorities such as CQC, to investigate ongoing risk?
Our observations
NHS Trusts and private health employers should monitor how many registrants they refer to the NMC as a performance indicator of culture and management style. The NMC needs to up its game in monitoring where referrals are coming from and intervening with employers who abuse the FtP process to intimidate and bully staff instead of competent empathic effective management.
Put simply:
- Trusts should be recording the number of registrants they refer to the NMC as a performance indicator and an indicator of culture and management style.
- If the NMC codes referrals from employers it could easily identify high referring trusts/boards/care companies where FTP referral is being misused.
- If the NMC continued with the employer link service this work could start to unpick shared themes between referrals to help identify potential links to poor care and patient groups at risk.
The process of gathering the data, and the quality and granularity of the data, further demonstrates to us the serious problems with the NMC and their regulation of fitness to practice processes. As long as there is a casual approach to data collection and a lack of willingness to share it publicly, FtP will remain a punitive, easily misused tool for employers and regulator. In turn, if the NMC embraced a willingness to serve patient safety more positively, then this could be the opportunity to do so, while also demonstrating a duty of care to their registrants and improving healthcare generally.
Wes Streeting are you listening?!
Credits:
FOIs and data gathering by Penny Ballinger.
Database, map and list © Peter C. Bell

Great work. I hope it is shared widely and read.
The number of nurses referred by NhS organisations is low in comparison to those referred by patients and relatives. That data is probably more important and needs to be collated in the same way.
Do we have more information on demographic detail, in particular any protected characteristics of those referred?
I’m afraid not at the moment – we have reached our limit of how many requests we can put into the NMC now so they are refusing all ongoing ones under section 12 – could you do a request and let us have the information when you receive it? email us support@nmcwatch.org.uk